The True Cost of Those ‘Free’ At-Home COVID Tests
By Damon Darlin | KHN
Americans keep hearing that it is important to test frequently for COVID-19 at home. But just try to find an “at-home” rapid COVID test in a store and at a price that makes frequent tests affordable.
Testing, as well as mask-wearing, is an important measure if the country ever hopes to beat COVID, restore normal routines and get the economy running efficiently. To get Americans cheaper tests, the federal government now plans to have insurance companies pay for them.
The Biden administration announced Jan. 10 that every person with private insurance can get full coverage for eight rapid tests a month. You can either get one without any out-of-pocket expense from retail pharmacies that are part of an insurance company’s network or buy it at any store and get reimbursed by the insurer.
Congress said private insurers must cover all COVID testing and any associated medical services when it passed the Families First Coronavirus Response Act and the CARES Act. The have-insurance-pay-for-it solution has been used frequently through the pandemic. Insurance companies have been told to pay for PCR tests, COVID treatments, and the administration of vaccines. (Taxpayers are paying for the cost of the vaccines themselves.) It appears to be an elegant solution for a politician because it looks free and isn’t using taxpayer money.
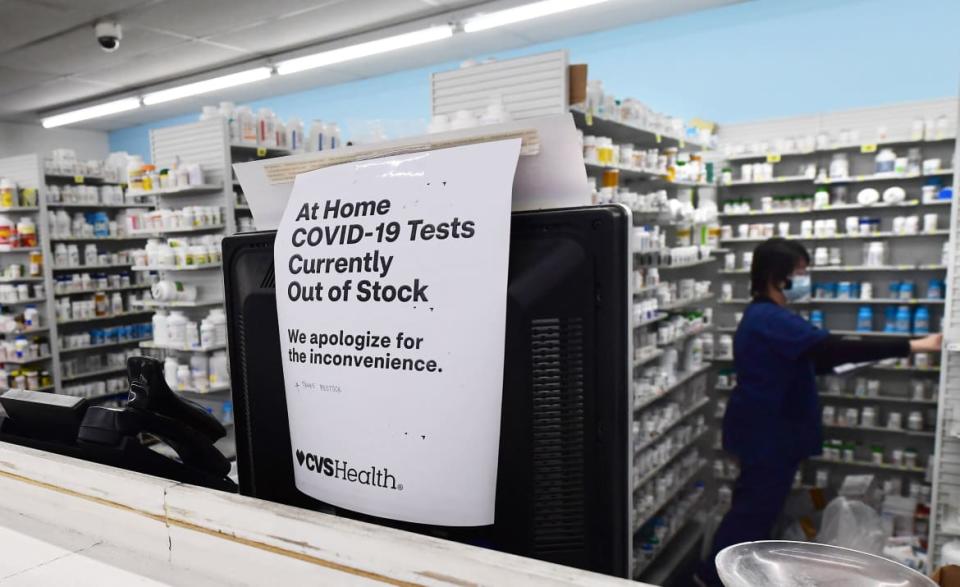
Good luck finding tests in stock, in stores, at a price low enough to make frequent use affordable.
Are the tests really free?
Well, no. As many an economist will tell you, there ain’t no such thing as a free lunch. Someone has to pick up the tab. Initially, the insurance companies bear the cost. Cynthia Cox, a vice president at KFF who studies the Affordable Care Act and private insurers, said the total bill could amount to billions of dollars. Exactly how much depends on “how easy it is to get them, and how many will be reimbursed,” she said.
Will the insurance company just swallow those imposed costs?
If companies draw from the time-tested insurance giants’ playbook, they’ll pass along those costs to customers. “This will put upward pressure on premiums,” said Emily Gee, vice president and coordinator for health policy at the Center for American Progress.
Major insurance companies like Cigna, Anthem, UnitedHealthcare and Aetna did not respond to requests to discuss this issue.
If that’s the case, why haven’t I been hit with higher premiums already?
Insurance companies had the chance last year to raise premiums but, mostly, they did not.
Why? Perhaps because insurers have so far made so much money during the pandemic they didn’t need to. For example, the industry’s profits in 2020 increased 41 percent to $31 billion from $22 billion, according to the National Association of Insurance Commissioners. The NAIC said the industry has continued its “tremendous growth trend” that started before COVID emerged. Companies will be reporting 2021 results soon.
The reason behind these profits is clear. You were paying premiums based on projections your insurance company made about how much health care consumers would use that year. Because people stayed home, had fewer accidents, postponed surgeries and, often, avoided going to visit the doctor or the hospital, insurers paid out less. They rebated some of their earnings back to customers, but they pocketed a lot more.
As the companies’ actuaries work on predicting 2023 expenditures, premiums could go up if they foresee more claims and expenses. Paying for millions of rapid tests is something they would include in their calculations.
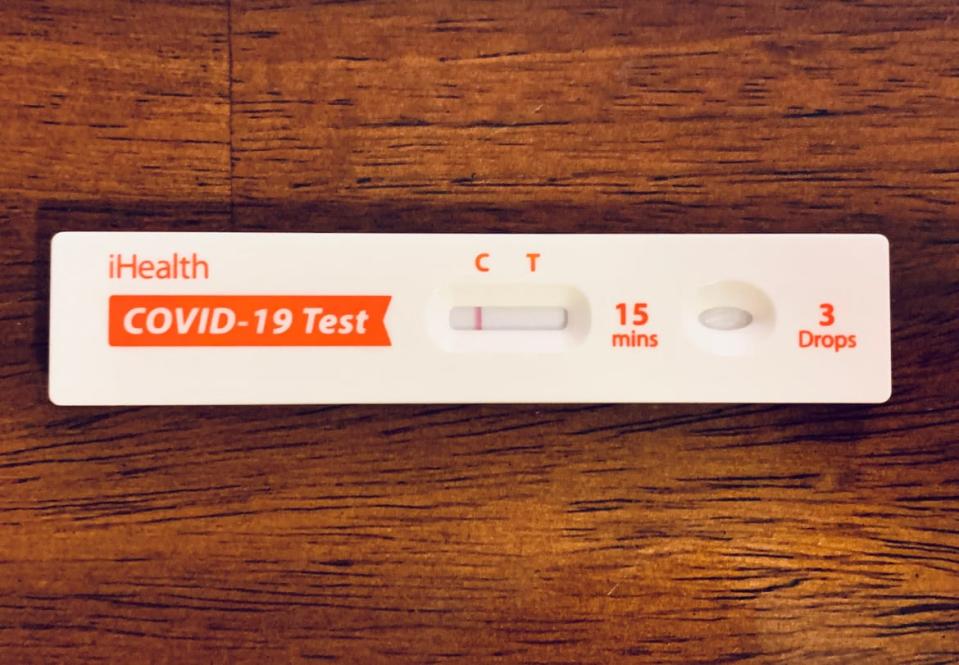
The insurance reimbursement is set at $12 per test, no matter how much you paid for yours.
Regardless of my premiums, will the tests cost me money directly?
It’s quite possible. If your insurance company doesn’t have an arrangement with a retailer where you can simply pick up your allotted tests, you’ll have to pay for them—at whatever price the store sets. If that’s the case, you’ll need to fill out a form to request a reimbursement from the insurance company. How many times have you lost receipts or just plain neglected to mail in for rebates on something you bought? A lot, right?
Here’s another thing: The reimbursement is set at $12 per test. If you pay $30 for a test—and that is not unheard of—your insurer is only on the hook for $12. You eat the $18.
And by the way, people on Medicare will have to pay for their tests themselves. People who get their health care covered by Medicaid can obtain free test kits at community centers.
A few free tests are supposed to arrive at every American home via the U.S. Postal Service. And the Biden administration has unveiled a website where Americans can order free tests from a cache of a billion the federal government ordered.
Will this help bring down the costs of at-home tests and make them easier to find?
The free COVID tests are unlikely to have much immediate impact on general cost and availability. You will still need to search for them. The federal measures likely will stimulate the demand for tests, which in the short term may make them harder to find.
But the demand, and some government guarantees to manufacturers, may induce test makers to make more of them faster. The increased competition and supply theoretically could bring down the price. There is certainly room for prices to decline since the wholesale cost of the test is between $5 and $7, analysts estimate. “It’s a big step in the right direction,” Gee said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Get the Daily Beast's biggest scoops and scandals delivered right to your inbox. Sign up now.
Stay informed and gain unlimited access to the Daily Beast's unmatched reporting. Subscribe now.

 money
money 