Here's what's gone wrong with US coronavirus testing, and how the 'logjam' can be broken
Coronavirus testing in the U.S., which lags other regions and is considered a linchpin to restarting the economy, has been mired with troubles since the onset of the pandemic — issues that are still a long way from being addressed.
As the White House pushes for a phased reopening in parts of the country, shortages of reagents and swabs— largely from China and Italy — are still an acute concern. The Centers for Disease Control was faulted early on for pushing faulty testing kits that contributed to the U.S.’s sluggish response to COVID-19, which has infected over 700,000 Americans and killed nearly 40,000.
The private sector is considered crucial to manufacturing the kits, but each company’s instrument has specific needs. Those barriers are creating stiff challenges to ramping up testing — particularly in New York, the epicenter of the U.S. outbreak.
“Testing is the single most important topic for us to understand, I think,” Gov. Andrew Cuomo said on Saturday, adding that labs continue to run into shortages of necessary supplies.
“We could actually be doing more if [companies] would give us the reagents,” Cuomo said, but supply chain woes in China have blocked efforts to scale quickly. “That's the logjam that we are in.”
Anthony Fauci, director of the National Institute for Allergy and Infectious Disease, said recently that “testing is...an important part of a multi-faceted way that we are going to control and ultimately end this outbreak,” but far from the only factor.
A ‘massive disconnect’
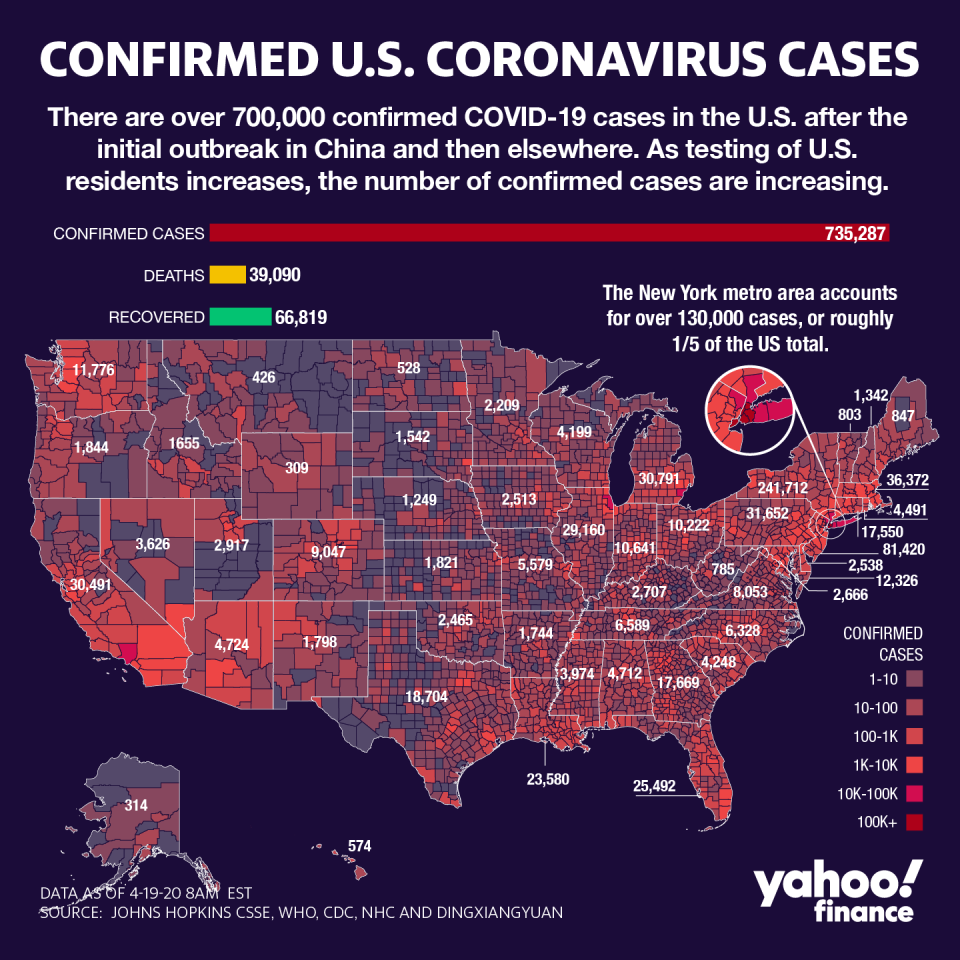
New York and New Jersey account for a majority of the deaths, and 45% of all cases in the country. The West Coast was able to reduce its spread with early mitigation tactics, but the NY-NJ metro area is now the center of the U.S. outbreak, largely because of testing problems.
Dr. Ashish Jha, director of Harvard University’s Global Health Institute, told Yahoo Finance that the outbreak requires daily or even weekly tracking to understand what is happening. However, without the proper equipment, the country is still flying blind.
“There is a massive disconnect between what we need and what we have,” Jha said.
The Empire State has done more testing than any of its counterparts, but needs a lot more in order to relax the severe lockdowns paralyzing its economy. However, there are promising developments with new types of kits that can be deployed in large amounts, and address the most vulnerable populations like African-Americans and Latinos. Including mobile testing sites, according to the task force this week.
It’s why 3D printing companies, as well as a new public-private partnership with the Gates Foundation, United Health Group (UNH) and U.S. Cotton, have all gotten involved. The coalition is promising more than 5 million swabs that will be sent to states, President Donald Trump said on Friday.
Dr. Deborah Birx, coordinator of the White House task force, has repeatedly said the country has enough high-volume testing capacity and “a team has been created to call every single laboratory and every single research institution across the United States to define the complete capacity in every single state.”
Yet there are wide gaps between the ability of states to process tests —and an even bigger political debate over testing scale, and who’s responsible for the delays. According to federal data, states like California, Florida, New York and Texas can complete 1 million tests per month; meanwhile Alaska, Hawaii, Oregon and West Virginia are only able to do 100,000 tests per month.
Some companies like Abbott (ABT) and Roche (RHHBY) have testing instruments that can process hundreds of results daily, but most Abbott instruments are located in hospitals and other dedicated health facilities, and most Roche instruments are in commercial labs.
Supply and demand

Commercial, public health and hospital laboratories have all hit similar roadblocks: They either lack the manpower or supplies to scale testing.
It’s also why some labs have announced furloughs and pulled 2020 guidance, amid an inability to meet the sudden demand spike of COVID-19 tests while seeing no demand for other testing. Meanwhile, agreements to waive cost-sharing have resulted in uneven payments.
“We know that the lack of predictable reimbursement for tests performed has been a barrier to entry for some laboratories...labs have been asked to do more with less,” the American Clinical Laboratory Association said recently.
Last month, the organization lobbied for inclusion in the $2.3 trillion economic stimulus package, citing the lopsidedness in non-coronavirus testing. To date, commercial lab giants like LabCorp (LH) and Quest Diagnostics (DGX) have completed the vast majority of COVID-19 testing, along with other ACLA member labs, totaling over 2 million of the 3.7 million-plus the U.S. has performed.
“The cost of supplies has increased, and laboratories are seeing a substantial decline in non-COVID-19 testing, as patient visits to physicians plummet and elective surgeries, screenings and routine care services are postponed,” the ACLA added.
By comparison, public health labs— which were early to the game but have slow turnaround times— completed less than 350,000, according to federal data. Hospital and academic labs, where Birx has been focused on ramping up capacity, have done more than half a million.
The Abbott ID NOW test, which can give results in under 15 minutes, has also run about half a million tests to-date, according to Admiral Brett Giroir, an assistant Health and Human Services Secretary assigned to the White House task force. Yet the solution is not cost-effective, because it can only do four tests per hour.
Birx said the country is working on ramping up different types of tests, including antigen and antibody tests, but even those are currently still in the works.
Harvard’s Jha said forward looking statements were fine, but with such sluggish results, the White House has a lot to prove.
“It shouldn’t be a national security secret of how much testing we are doing,” he said.
[Click here for more of Yahoo Finance’s coronavirus coverage: Personal finance tips, news, policy, graphics & more from Yahoo Finance]
Anjalee Khemlani is a reporter at Yahoo Finance. Follow her on Twitter: @AnjKhem
Follow Yahoo Finance on Twitter, Facebook, Instagram, Flipboard, LinkedIn, and reddit.
Find live stock market quotes and the latest business and finance news

 money
money 
